4/24/2015
We do not diagnose disease or recommend a dietary supplement for the treatment of disease. You should share this information with your physician who can determine what nutrition, disease and injury treatment regimen is best for you. You can search this site or the web for topics of interest that I may have written (use Dr Simone and topic).
“We provide truthful information without emotion or influence from the medical establishment, pharmaceutical industry, national organizations, special interest groups or government agencies.” Charles B Simone, M.MS., M.D.
AB BLOOD TYPE INCREASES RISK FOR HEART DISEASE

Lawrenceville, NJ (Dr Simone) – People with blood types A, B, or AB have a greater risk for developing coronary heart disease and autoimmune disease when compared to those with blood type O.
Blood type AB – 4% of the population – 23% increased risk
Blood type B – 12% of population – 11% increased risk
Blood type A – 36% of population – 5% increased risk
The findings are based on an analysis of 62,073 nurses in the Nurses Health Study and 27,428 adults in the Health Professional Follow-up Study. These people were predominantly white, aged 30-75 and followed for at least 20 years.
The mechanism for this increased risk seems to be a genetic inheritance of a non-O blood group. In non-O individuals, plasma levels of clotting factor VIII-von Willebrand factor (vWF) complex are ≈25% higher than group O individuals which confers higher risk.
Several anticoagulants can interfere with the clotting factor VIII-von Willebrand Factor (vWF) complex, either directly or indirectly. Here’s a breakdown of some of the key anticoagulants and how they might affect this complex:
-
Heparin –
-
Unfractionated Heparin (UFH) and Low Molecular Weight Heparin (LMWH):
-
These anticoagulants do not directly affect factor VIII or vWF, but they do enhance the activity of antithrombin III which inhibits several clotting factors, including factor Xa and IIa (thrombin). Since thrombin activates factor VIII, indirectly, heparin can influence the function of factor VIII by reducing thrombin generation. However, heparin does not directly degrade or inhibit factor VIII or vWF.
-
Direct Thrombin Inhibitors (e.g., Dabigatran):
-
By inhibiting thrombin, these drugs reduce the activation of factor VIII, thereby affecting the clotting process where factor VIII is involved.
-
Vitamin K Antagonists (like Warfarin):
-
Warfarin does not directly inhibit factor VIII or vWF, but by reducing the synthesis of vitamin K-dependent clotting factors (II, VII, IX, and X), it can influence the overall clotting cascade where factor VIII is involved.
-
Direct Factor Xa Inhibitors (e.g., Rivaroxaban, Apixaban, Edoxaban):
-
These drugs inhibit factor Xa, which is upstream in the coagulation cascade from factor VIII activation. Their primary action isn’t on factor VIII-vWF, but they do affect the thrombin generation necessary for factor VIII activation.
-
Von Willebrand Factor Inhibitors (e.g., Caplacizumab):
-
Caplacizumab is a relatively new drug specifically targeting vWF for the treatment of acquired thrombotic thrombocytopenic purpura (TTP). It directly inhibits vWF and hence impacts the function of the factor VIII-vWF complex.
Other studies show that non-O individuals have higher lipid levels (cholesterol, triglycerides) and inflammatory markers, including soluble intercellular adhesion molecule, plasma soluble E-selectin levels, P-selectin levels, and tumor necrosis factor-α.
All of these elevated levels of inflammation increase the risk for coronary heart disease.
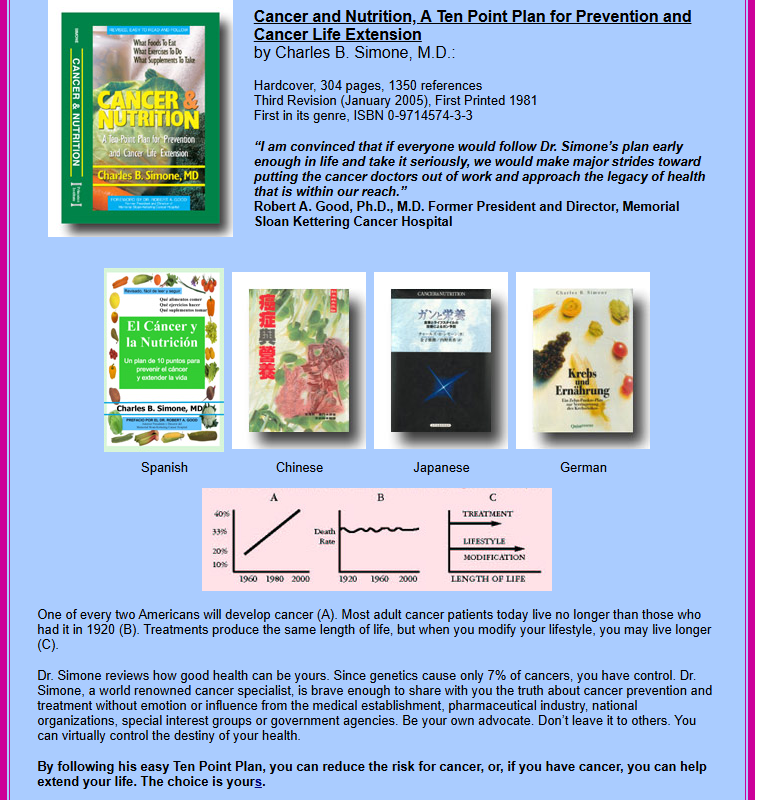
You can’t change your blood type, but you can decrease your risk by adhering to a healthy lifestyle as per our Ten Point Plan
(c) 2017 Charles B. Simone, M.MS., M.D.